Obesity: A Disease
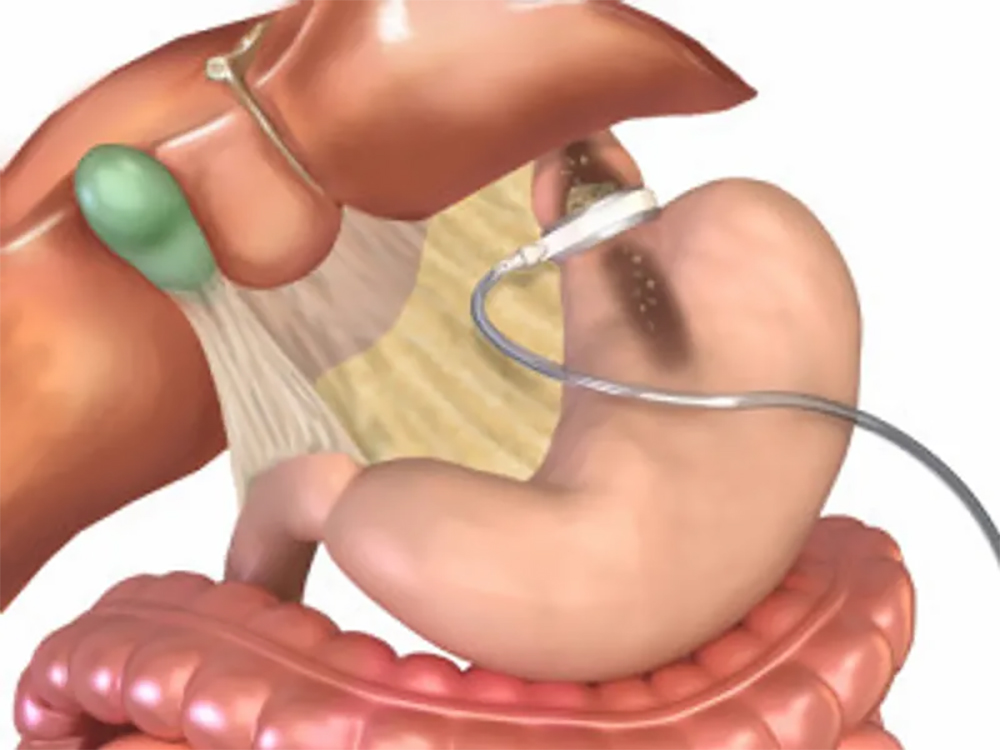
Laparoscopic Adjustable Silicone Banding with the LAP-BAND’ has proven to be a safe Bariatric surgical procedure. It is minimally invasive, adjustable and easily reversible. It does not involve rerouting or rearranging of the intestines. It does not involve dividing the gastrointestinal tract, and therefore it involves no staple lines. It is a purely restrictive procedure, and thus, does not involve any malabsorption. The operative time is among the shortest of Bariatric procedures, and the length of hospital stay is usually one night. This procedure has also been proven to be one. of the safest operations, with a mortality rate of approximately I in 2,000. This is about one-tenth the mortality rate of gastric bypass’. It works because patients eat less and have a sense of fullness, otherwise known as a sense of satiety. The procedure was first introduced by BelacheW2 in 1993. There have been more than 100,000 of these surgeries performed to date.
Living with the LAP-BAND presents unique lifestyle adjustments and challenges. We will provide an overview of the dietary guidelines, role of exercise, and adjustment schedule. It cannot be overemphasized that the LAP-BAND is a purely restrictive model for weight loss. This is in stark contrast to both the Roux-en-Y Gastric Bypass and the Duodenal Switch which involve a malabsorptive component to the operation.
Comparing weight loss from a LAP-BAND to either of these operations is like comparing apples to oranges. The first rule in living and thriving with the LAP-BAND is to remember that the weight loss is slow and gradual. Weight loss in the range of 1-2 lbs. per week is considered successful. A common source of disappointment and frustration comes when a LAP-BAND patient compares his or her weight loss to a sibling or coworker who has had a gastric bypass. Patience and understanding are critical components to success with the LAP-BAND.
Treatment Options
Non-Surgical Treatment Options for Morbid Obesity
Non-Surgical Treatment Dieting, exercise, and medication have long been regarded as the conventional methods to achieve weight loss. Sometimes, these efforts are successful in the short term. However, for people who are morbidly obese, the results rarely last. For many, this can translate into what’s called the “yo-yo syndrome,” where patients continually gain and lose weight with the possibility of serious psychological and health consequences. Recent research reveals that conventional methods of weight loss generally fail to produce permanent weight loss. Several studies have shown that patients on diets, exercise programs, or medication are able to lose approximately 10% of their body weight but tend to regain two-thirds of it within one year, and almost all of it within five years.(1) Another study found that less than 5% of patients in weight loss programs were able to maintain their reduced weight after five years.(2)
Surgical Treatment Options for Morbid Obesity
Surgical Treatment Over the years, weight-loss surgery has proven to be a successful method for the treatment of morbid obesity.3 Surgical options have continued to evolve and Heartland Surgical Associates is pleased to be able to offer patients the LAP-BAND¨ System surgery. This procedure is the safest, least traumatic and only adjustable and reversible obesity surgery available in the United States. The LAP-BAND System provides a unique tool that can help you achieve and maintain significant weight loss, improve your health, and enhance your quality of life.
1. American Association of Clinical Endocrinologists (AACE) / American College of Endocrinology (ACE) Statement on the Prevention, Diagnosis, and Treatment of Obesity (1998 Revision). AACE/ACE Obesity Task Force. Endocr Pract. 1998; Vol. 4 No. 5: 297-330. 2. Kramer FM et al. Long-term follow-up of behavioral treatment for obesity: patterms of weight regain among men and women. Int J Obes 1989; 13:123-136. 3. SAGES/ASBS Guidelines for Laparoscopic and Conventional Surgical Treatment of Morbid Obesity. American Society for Bariatric Surgery. http://asbs.org/html/guidelines.html LAP-BAND¨ System Overview
Approved by the FDA in June 2001, LAP-BAND System is the safest, least invasive and only adjustable surgical treatment for morbid obesity in the United States. It induces weight loss by reducing the capacity of the stomach, which restricts the amount of food that can be consumed. Since its clinical introduction in 1993, almost 150,000 LAP-BAND procedures have been performed around the world and over 30,000 in the U.S. alone.